LGBT Indians want ‘discriminatory’ blood donation ban lifted

 Getty Images
Getty ImagesIn 2018, India’s highest court legalized gay sex in a landmark ruling – but the country still does not allow transgender and bisexual men to donate blood.
People from the LGBT community say the decades-old ban is “discriminatory” and have gone to court to challenge it.
When Vyjayanti’s mother Vasanta Mogli was on her deathbed battling advanced Parkinson’s, she needed regular blood transfusions.
But Ms Mogli, a transgender woman based in the southern city of Hyderabad, could not donate blood despite being the sole carer of her mother.
“I had to keep posting [requests for blood donors] on WhatsApp and Facebook groups,” he said, describing the process as “torturous”.
Ms. Mogli was lucky enough to find sponsors for her mother but many others did not.
Beoncy Laisharam – a doctor in the northeastern state of Manipur – recounts the experience of one of her patients, whose transgender daughter was unable to donate blood for treatment.
“My father needed two to three units of blood a day. They couldn’t get blood from other sources,” she said.
“He died two days after being admitted.”
It was such news that forced Sharif Ragnerka, a 55-year-old writer and activist, to file a petition in the Supreme Court of India against the ban on blood donation by LGBT people.
Indian laws prevent LGBT people from donating blood on the grounds that they are at high risk of HIV-Aids – it is mandatory that donors are free from transfusion-transmitted diseases.
This policy dates back to the 1980s, when several countries imposed similar restrictions to control the global HIV-Aids epidemic, which killed thousands.
Despite the change in attitude, subsequent policies have kept the ban in place, including the latest law drafted in 2017.
Filed in July, the petition says the current blood donation policies are “extremely discriminatory and arbitrary” and violate the fundamental rights to “equality, dignity and life” of the LGBT community.
The court asked the federal government to respond to Mr. Ragnerka’s request and include two similar court cases filed in 2021 and 2023 pending.
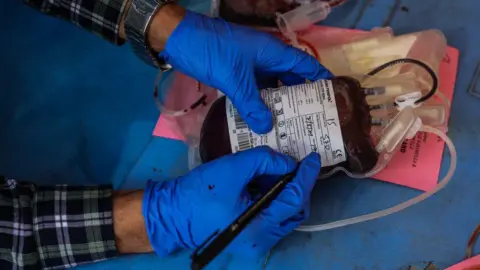 Getty Images
Getty ImagesIn a previous case, the government defended the ban by citing a 2021 health ministry report that said transgender, gay and bisexual men were “six to 13 times more likely” to contract HIV than the general population.
“The government’s mission is to reduce risk without moral judgment [attached to] with it,” said Dr. Joy Mammen, a blood transfusion specialist.
But critics say the policy is racist, entrenched in discrimination and makes them feel “left out and insignificant”.
“Other sexes also have people with HIV but their whole society is not closed [from donating blood],” said Dr. Beoncy, adding that the ban reinforces existing ideas.
India is home to tens of millions of LGBT people. In 2012, the Indian government put the population at 2.5 million, but global estimates suggest the actual number may be more than 135 million.
Many of them faced discrimination and were forced to leave their families.
Campaigners say the ban hampers their access to essential health care as it prevents them from taking blood from their partners or “chosen families”.
“If there is a total ban on blood donation by LGBT people, how do you expect members of the public to get help in emergencies?” asked Sahil Choudhary, an LGBT activist.
In many cases, donors may also feel compelled to lie about their gender while filling out a mandatory form to donate blood, in order to save the life of a loved one.

Activists say that apart from this being discriminatory, the ban is unreasonable and due to the huge need for blood transfusions in the country.
A learn published by the Public Library of Science in 2022 estimated that India faced an annual shortage of nearly one million units of blood.
Thangjam Santa Singh, a transgender rights activist who filed a lawsuit against the ban last year, said India’s current laws are outdated as several countries have moved away from restrictions on LGBT blood donors in recent years.
Last year, the US lifted all restrictions on gay men and men and women donating blood. Now instead of choosing a gender, donors are screened on the basis that they have engaged in “high risk sexual behaviour”.
All potential donors must answer a questionnaire about their recent sexual history. Those who have had a new sexual partner, have multiple sexual partners and have had anal sex in the past three months are asked to wait three months before donating blood.
The reason is that new testing technology allows rapid detection of HIV cases, so potential donors can give blood safely based on an individual risk assessment.
The UK set similar guidelines in 2021. Other countries have lifted the ban or eased restrictions, including Brazil, the Republic of Ireland, Canada, France and Greece.
The petitioners argued that India should also have an individualized blood donation system based on “actual risk” and not “perceived risk”.
 Getty Images
Getty ImagesMs Singh said the Indian government could consider deferring based on a donor’s recent sexual history, instead of denying the entire LGBT community the opportunity to donate altogether.
“This makes me feel like I’m not human,” she said.
The Indian government has opposed this, saying that the country’s health system is not ready for change.
In its response to earlier petitions filed in the Supreme Court, the federal government had said advanced blood testing methods, such as nucleic-acid testing widely used in other countries, were only available in “a small proportion” of blood banks. in India.
“In India, the systems are not strong enough,” said Dr Mammen.
This applies not only to “testing” but also to “ensuring an environment where there is privacy and confidentiality so that people feel comfortable answering questions about their sexual history,” he added.
But members of the public are not convinced – and say they will continue to fight the “discriminatory ban”.
“I always think about how I won’t be able to donate blood to my family if there is an urgent need,” said Mr. Ragnerka.
“I don’t want to spend the rest of my life trying to find ways to deal with these problems.”
Source link




